Two possible mistakes
Every day, doctors have to make decisions without the benefit of a large randomized-controlled trial (RCT) to guide their every move. That’s a normal part of medicine.
Whenever I am conflicted about whether or not to start a treatment, I think about two possible mistakes I could make: I could give a patient a treatment they don’t need or I could withhold a treatment they do need. I then try to gauge both how consequential and how probable each mistake might be. For someone with a potentially dangerous condition that has a safe treatment, it’s better to overtreat several patients than to undertreat just one.
In a nationwide cohort of more than 1 million adults aged 65 years and older, no increased risk of 28 adverse events was observed following vaccination with a monovalent XBB.1.5-containing vaccine.
Let’s apply this thinking with the updated COVID vaccine. (It shouldn’t be called a booster, though I will do so for the sake of simplicity). There are two possible mistakes. You could give someone a booster they don’t need or you could withhold a booster from someone who needs it.
Right away, it’s obvious the risks are not symmetric. Beyond a sore arm and fever, harms from the booster are mercifully rare. Vaccine-myocarditis occurs mainly adolescent males (1 in 15,000 to 1 in 88,000) and is universally described as “mild” by the doctors who treat it. The booster seems totally safe for older people who need it the most. According to one study from February 2024:
In a nationwide cohort of more than 1 million adults aged 65 years and older, no increased risk of 28 adverse events was observed following vaccination with a monovalent XBB.1.5-containing vaccine.
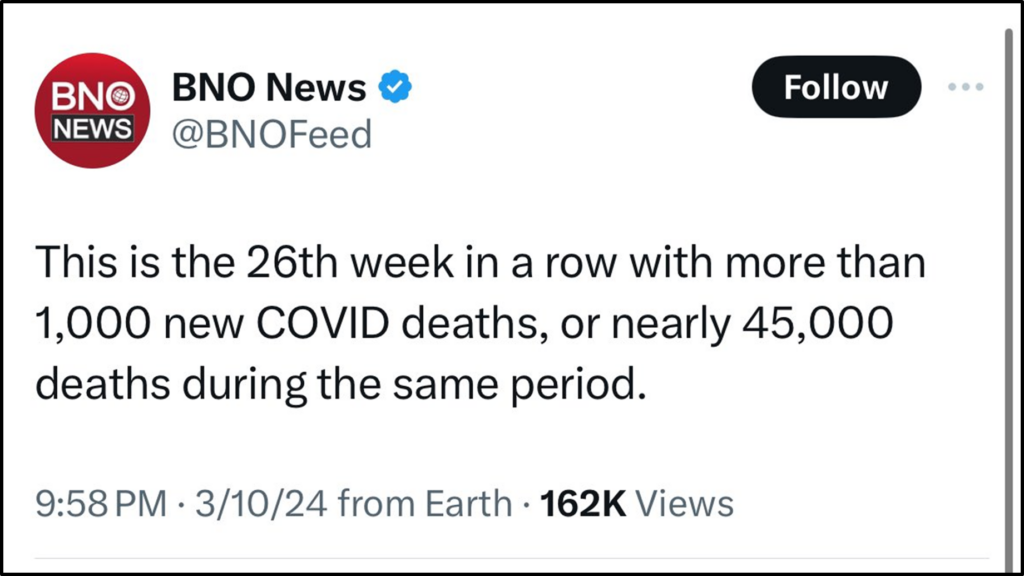
In contrast, COVID continues to kill and disable people.
Withholding a needed booster, especially from an older, vulnerable person, is clearly more consequential than giving someone a booster they don’t need.
If the U.S. moved at a faster pace to approve it and get people boosted, an estimated 29,000 lives could have been saved.
Next, we need to know how probable it is that boosters reduce COVID’s harms. There was a RCT for the first booster, showing “95.3% efficacy against Covid-19 as compared with two doses”, though this impressive result didn’t stop some doctors from trashing this dose. As the pandemic progressed and knowledge accumulated, scientists reasonably concluded that it wasn’t necessary to start over at step 1 and do an RCT for every tweak to the vaccine. RCTs are slow, the virus spreads quickly, and there’s a real cost to waiting.
Of course, it wasn’t totally absurd to believe that a vaccine that generated a strong immune response against SARS-CoV-2 would also protect against COVID itself. Other vaccines have been approved based on immunogenicity without controversy, and one meta-analysis from March 2023 found:
Predicted neutralising antibody titres are strongly correlated with observed vaccine effectiveness against symptomatic and severe COVID-19
Indeed, nearly 60 observational studies (see below) as well as several systematic reviews and meta-analyses have shown that boosters limit COVID’s harms, though they are not a panacea and their benefit wanes quickly. Other studies have shown that boosters limit viral transmission.
Maybe it’s true that every one of these studies is “plagued by confounding” and totally useless, as some doctors claim. Maybe it’s just a statistical fluke that they all point in the same direction. If that’s the case, millions of people got sore arms for no reason and a small number of young men got “mild” myocarditis. That’s definitely not a good thing, but it’s a drop in the bucket compared to COVID’s toll.
But what if these studies were not entirely a statistical fluke? What if they were right, and the booster actually keeps some people alive and out of the hospital? It’s not absurd to believe this, is it? Then, it would be a huge mistake to deprive someone of a booster dose they needed. Indeed one modeling study estimated:
That through June 2022, if the U.S. moved at a faster pace to approve it and get people boosted, an estimated 29,000 lives could have been saved.
Looking at all the evidence, I am confident that more people suffered grave injuries from missing a needed dose than from getting an unneeded dose. That’s likely to be the case moving forward as well. COVID isn’t going anywhere, and while deaths are much lower than before, over 1,000 Americans are still dying of COVID every week, and many more are being injured by it. It seems neither terrible nor scientifically implausible to try blunt COVID’s harms with a periodic booster, even one that hasn’t proven its value in a large and lengthy RCT.
They are net harmful- due to AEs (adverse events) at time of injection.
Many doctors disagreed with this. They felt, unless every modification to the vaccine had proven its value via a massive RCT, then one could assume the vaccine did not work. These doctors could never show the vaccine was dangerous, especially for older people who needed it the most. It seems OK to get 217 vaccines. However, they felt the data supporting the vaccine just wasn’t robust enough, and from that, they took a massive leap and concluded we should just the virus repeatedly infect everyone. There was nothing we could do about it. We want them infected wasn’t just for young people anymore. It was for everyone.
For some, this was literally a religious belief. Data-trickster Florida Surgeon General Dr. Joseph Ladapo recently issued a statement titled Florida State Surgeon General Calls for Halt in the Use of COVID-19 mRNA Vaccines. He also told Steve Bannon:
I think it probably does have some integration at some levels with the human genome because these vaccines are honestly—they’re the Antichrist of all products.
Other doctors fundamentally agreed with Dr. Ladapo. They ridiculed and shamed anyone, including older, vulnerable people, who wanted even the first booster, the one with RCT-data supporting it. One doctor, who previously claimed post-vaccination fevers- “we’re talking about grade three fevers!“- was a valid reason to let unvaccinated children contract COVID, gave sore arms as his key reason why we should let unboosted seniors contract COVID. He said:
They are net harmful- due to AEs (adverse events) at time of injection.
This doctor, seeking to encourage conformity and groupthink amongst his paying followers, even asked them to sign a pledge to refuse booster doses, a classic influencer technique.
Because of subsequent increasing incidence, more and more boosters were added to compensate for “waning immunity” and now children get 6 doses by 6 years old.
None of this was new.
As those of us who cared about vaccines before the pandemic know very well, anti-vaxxers have long claimed that mundane vaccine-side effects are worse than the diseases they prevent. For example, prior to the pandemic germ-theory denier Dr. Kelly Brogan discouraged the flu vaccine by writing:
Common side effects include symptoms like fatigue, fever, body and headaches (aka…the flu!)
Obviously, these side effects are not the same as getting the flu itself, which can kill children especially unvaccinated ones.
Additionally, anti-vaxxers have long tried to scare parents based on the number of vaccines children receive and literally nothing else. “Too many, too soon” is the unofficial slogan of the anti-vaccine movement. Anti-vaxxers think is clever to simply state the number of vaccine doses, often paired with a frightening image of syringes in a baby doll, as if that number alone is a strike against vaccines. For example, prior to the pandemic, Dr. Brogan encouraged parents to leave their children vulnerable to whooping cough by saying:
Because of subsequent increasing incidence, more and more boosters were added to compensate for “waning immunity” and now children get 6 doses by 6 years old.
She’s right that kids get the DTaP multiple times, but this is not a valid argument against this vaccine. It’s a scare tactic. Yet, respectable doctors copied Dr. Brogan’s rhetoric during the pandemic to spread doubt about the COVID booster- I, like many of my patients, have questions about the 7th, 8th, and 9th booster (I wish I was exaggerating). Of course, anyone who survived long enough to get their 9th booster is doing something right.
Getting COVID is inevitable. It is just another cold or flu like illness.
In a pandemic where over a million Americans died and millions more were injured- many of them unvaccinated or undervaccinated– some doctors, aided by a prominent vaccine hero, put forth enormous effort to discourage boosters. As an alphabet soup of immune-evading variants invalidated their 2021 declarations that the initial two vaccine doses would end the pandemic, these doctors responded not by humbly acknowledging they initially overhyped vaccines and underestimated the virus, but rather by trashing subsequent vaccine doses, even for older, vulnerable people.
This is where they spent their time and energy. This is how they chose to use their privileged voice as trusted doctors. This was the hill they were willing to die on.
There was nothing unique about the campaign against boosters, but it was very revealing. It was just a small part of a pathetic, pandemic-long pattern where doctors expressed grave concern about the mildest harms of measures to limit COVID, even mere abnormal lab values, while being totally indifferent to literally anything the virus could do, including the deaths of children and young adults.
Like the inexorable passage of time, some doctors treated the virus as a totally unmodifiable force – Repeat infections are inevitable. More the longer you live. Nothing can be done about it. Getting COVID is inevitable. It is just another cold or flu like illness. By claiming- falsely– that COVID was just another cold or flu and that “nothing” that could be done about it anyways, they gave themselves permission to breezily brush away its harms. Indeed, the same doctor who fretted mightily about “grade three fevers” in vaccinated children and “AEs at time of injection” also said we should accept children dying of COVID “as a matter of course” and there are zero “smart people who still give a shit about COVID.”
Put another way, some doctors cared much more about sore arms than cold bodies.
Observational Studies of the COVID Booster
- Barda (2021): Vaccine effectiveness evaluated at least 7 days after receipt of the third dose, compared with receiving only two doses at least 5 months ago, was estimated to be 93% (231 events for two doses vs 29 events for three doses; 95% CI 88–97) for admission to hospital, 92% (157 vs 17 events; 82–97) for severe disease, and 81% (44 vs seven events; 59–97) for COVID-19-related death.
- Arbel (2021): Participants who received a booster at least 5 months after a second dose of BNT162b2 had 90% lower mortality due to Covid-19 than participants who did not receive a booster.
- Bar-on (2021): Across the age groups studied, rates of confirmed Covid-19 and severe illness were substantially lower among participants who received a booster dose of the BNT162b2 vaccine than among those who did not.
- Muhsen (2022): The results of this cohort study suggest that receipt of a fourth BNT162b2 dose conferred high protection against COVID-19 hospitalizations and deaths among long-term care facilities residents during a substantial Omicron variant surge, but protection was modest against infection.
- Thompson (2022): During both Delta- and Omicron-predominant periods, receipt of a third vaccine dose was highly effective at preventing COVID-19–associated emergency department and urgent care encounters (94% and 82%, respectively) and preventing COVID-19–associated hospitalizations (94% and 90%, respectively).
- Andrews (2022): Against hospitalization or death, absolute effectiveness of a BNT162b2 booster ranged from around 97% to 99% in all age groups irrespective of the primary course, with no evidence of waning up to 10 weeks.
- Menni (2022): Vaccine effectiveness for booster doses in 0–3 months after BNT162b2 primary vaccination was higher than 92·5%, and effectiveness for heterologous boosters after ChAdOx1 nCoV-19 was at least 88·8%.
- Abu-Raddad (2022): Booster effectiveness against Covid-19–related hospitalization and death due to omicron infection, as compared with the primary series, was 76.5% (95% CI, 55.9 to 87.5). BNT162b2 booster effectiveness against symptomatic infection with the delta (or B.1.617.2) variant, as compared with the primary series, was 86.1%
- Moreira (2022): A third dose of the BNT162b2 vaccine administered a median of 10.8 months after the second dose provided 95.3% efficacy against Covid-19 as compared with two doses of the BNT162b2 vaccine during a median follow-up of 2.5 months.
- Klein (2022): Two doses protect against COVID-19–associated emergency department and urgent care encounters among children and adolescents. However, vaccine effectiveness (VE) was lower during Omicron predominance and decreased with time since vaccination; a booster dose restored VE to 81% among adolescents aged 16–17 years. Overall, 2-dose VE against COVID-19–associated hospitalization was 73%–94%.
- Regev-Yochay (2022): Vaccine efficacy was estimated to be higher for the prevention of symptomatic disease (43% for BNT162b2 and 31% for mRNA-1273)…Our data provide evidence that a fourth dose of mRNA vaccine is immunogenic, safe, and somewhat efficacious (primarily against symptomatic disease).
- Mallah (2022): A booster dose of COVID-19 vaccine increases the protection against SARS-CoV-2 infection and COVID-19 severity in the general population and in comorbid patients.
- Magen (2022): Relative vaccine effectiveness in days 7 to 30 after the fourth dose was estimated to be 45% (95% confidence interval [CI], 44 to 47) against polymerase-chain-reaction–confirmed SARS-CoV-2 infection, 55% (95% CI, 53 to 58) against symptomatic Covid-19, 68% (95% CI, 59 to 74) against Covid-19–related hospitalization, 62% (95% CI, 50 to 74) against severe Covid-19, and 74% (95% CI, 50 to 90) against Covid-19–related death.
- Adams (2022): During the first six months of 2022 in the US, booster doses of a covid-19 vaccine provided additional benefit beyond a primary vaccine series alone for preventing hospital admissions with omicron related covid-19.
- Tenforde (2022): Bivalent booster doses provided additional protection against COVID-19–associated emergency department/urgent care encounters and hospitalizations in persons who previously received 2, 3, or 4 monovalent vaccine doses. Because of waning of monovalent vaccine-conferred immunity, relative effectiveness of bivalent vaccines was higher with increased time since the previous monovalent dose.
- Tai (2022): This study found that in a young, healthy, highly vaccinated cohort frequently monitored for SARS-CoV-2, booster vaccination was associated with a significant reduction in incident infections during the Omicron wave.
- Ng (2022): Estimated mRNA booster effectiveness against severe COVID-19 was 87.4% with no evidence of waning up to 6 months after boosting, while the estimated 3-dose inactivated SARS-CoV-2 booster effectiveness against severe COVID-19 was 69.6%. Booster mRNA vaccine protection against severe COVID-19 was estimated to be durable over 6 months.
- Ridgway (2022): In a large US population, mRNA boosters were associated with decreased odds of hospitalization compared with the mRNA vaccine primary series alone, with the magnitude of the association attenuated with more time since the booster dose.
- Lauring (2022): mRNA vaccines were found to be highly effective in preventing covid-19 associated hospital admissions related to the alpha, delta, and omicron variants, but three vaccine doses were required to achieve protection against omicron similar to the protection that two doses provided against the delta and alpha variants.
- McConeghy (2022): In this cohort study of 10 949 residents of 202 community nursing homes and 4321 residents of 128 Veterans Health Administration community living centers, booster vaccination was associated with significant reductions in SARS-CoV-2 infections, hospitalizations, and the combined end point of hospitalizations or deaths.
- Accorsi (2022): These findings suggest that vaccination with 3 doses of mRNA COVID-19 vaccine, compared with being unvaccinated and with receipt of 2 doses, was associated with protection against both the Omicron and Delta variants, although higher odds ratios for the association with Omicron infection suggest less protection for Omicron than for Delta.
- Spitzer (2022): Among health care workers previously vaccinated with a 2-dose series of BNT162b2, administration of a booster dose compared with not receiving one was significantly associated with a lower rate of SARS-CoV-2 infection in short-term follow-up.
- Kelly (2022): In a US cohort of patients receiving care at Veterans Health Administration facilities during a period of Delta and Omicron variant predominance, there was a low incidence of hospitalization with COVID-19 pneumonia or death following vaccination and booster with any of BNT162b2, mRNA-1273, or Ad26.COV2.S vaccines.
- Surie (2022): Among immunocompetent adults aged ≥65 years hospitalized in the multistate IVY Network, a bivalent booster dose provided 73% additional protection against COVID-19 hospitalization compared with past monovalent mRNA vaccination only.
- Fleming-Dutra (2022): Among children and adolescents, estimated vaccine effectiveness for 2 doses of BNT162b2 against symptomatic infection decreased rapidly, and among adolescents increased after a booster dose.
- Johnson (2022): IRRs and VE were higher among persons who were fully vaccinated and had received a booster dose than among fully vaccinated persons who had not received a booster dose for cases and deaths during the period of Delta predominance and for cases during the period of Omicron emergence in December. The added benefits of booster doses were especially prominent among persons aged 50–64 and ≥65 years.
- Grewal (2022): The findings suggest that compared with a third dose of mRNA covid-19 vaccine, a fourth dose improved protection against infection, symptomatic infection, and severe outcomes among long term care residents during an omicron dominant period. A fourth vaccine dose was associated with strong protection against severe outcomes in vaccinated residents compared with unvaccinated residents, although the duration of protection remains unknown.
- Danza (2022): During both Delta and Omicron predominance, incidence and hospitalization rates were highest among unvaccinated persons and lowest among vaccinated persons with a booster.
- McConeghy (2022): In a large cohort of nursing home residents, receipt of a second mRNA COVID-19 booster dose during circulation of SARS-CoV-2 Omicron subvariants was 74% effective at 60 days against severe COVID-19–related outcomes (including hospitalization or death) and 90% against death alone compared with receipt of a single booster dose.
- Roberts (2022): COVID-19 vaccines were highly protective against infection and severe COVID-19 resulting in hospitalization, intensive care unit admission, or death. Administration of a booster dose significantly increased vaccine effectiveness against both outcomes.
- Gazit (2022): A fourth dose of the BNT162b2 vaccine appears to have provided additional protection against both SARS-CoV-2 infection and severe covid-19 disease relative to three vaccine doses. However, relative effectiveness of the fourth dose against infection appears to wane sooner than that of the third dose.
- Wei (2023): Overall vaccine effectiveness against death at 4 to 6 months after the third dose was greater than 90% for CoronaVac, BNT162b2, and the mixed vaccine schedule. While vaccines were generally estimated to be effective against severe outcomes caused by SARS-CoV-2 Omicron infection, this analysis found that protection in older patients was more likely to wane 6 months after the second dose. Hence, a booster dose is recommended for older patients to restore immunity.
- Lundberg-Morris (2023): Vaccine effectiveness against post-covid-19 condition for one dose, two doses, and three or more doses was 21%, 59%, and 73%, respectively.
- Finci (2023): Among Albanian healthcare workers, most of whom had been previously infected, COVID-19 booster dose offered improved VE during a period of Omicron BA.1 and BA.2 circulation.
- Wong (2023): Among nursing home residents who were up to date with COVID-19 vaccination (most had received a bivalent vaccine), vaccine effectiveness against SARS-CoV-2 infection was 31.2%.
- Klein (2023): BNT162b2 protected children and adolescents against mild to moderate and severe COVID-19. VE was lower during Omicron predominance including BA.4/BA.5, waned after dose 2 but increased after a monovalent booster.
- Link-Gelles (2023): A bivalent mRNA booster dose provided additional protection against symptomatic XBB/XBB.1.5 infection for at least the first 3 months after vaccination in persons who had previously received 2–4 monovalent vaccine doses.
- Andersson (2023): Heterologous booster schedules are associated with increased protection against severe, omicron related covid-19 outcomes compared with primary course schedules and homologous booster schedules.
- Andersson (2023): Vaccination with bivalent BA.4-5 or BA.1 mRNA booster vaccines as a fourth dose was associated with reduced rates of covid-19 related hospital admission and death among adults aged ≥50 years.
- Stecher (2023): Our results indicate an increased protective effect of a fourth dose against severe outcomes compared with a third dose, with decreasing effect with time since the last dose.
- Link-Gelles (2023): In this case-control study of COVID-19 vaccines and illness, VE associated with protection against medically attended COVID-19 illness was lower with increasing time since last dose; estimated VE was higher after receipt of 1 or 2 booster doses compared with a primary series alone.
- Lin (2023): Although the two bivalent vaccines were designed to target the BA.4–BA.5 subvariants, they were also associated with a lower risk of infection or severe infection with the BQ.1–BQ.1.1 and XBB–XBB.1.5 subvariants. The effectiveness was higher against hospitalization and death than against infection and waned gradually from its peak over time.
- Lin (2023): Vaccine effectiveness against severe infection resulting in hospitalization or death was 24.9% (95% CI, 1.4 to 42.8) for one monovalent booster dose and 61.8% (95% CI, 48.2 to 71.8) for one bivalent booster dose.
- Jang (2023): The 4-dose booster, irrespective of history of SARS-CoV-2 infection, was associated with higher protection against critical BA.5 infection, as shown in previous studies.
- Arbel (2023): Participants who received a bivalent mRNA booster vaccine dose had lower rates of hospitalisation due to COVID-19 than participants who did not receive a bivalent booster vaccination, for up to 120 days after vaccination. These findings highlight the importance of bivalent mRNA booster vaccination in populations at high risk of severe COVID-19
- Lewis (2023): Vaccine booster doses increased protection against COVID-19 hospitalization compared with a primary series.
- Tartof (2023): A BNT162b2 BA.4/5 bivalent booster restored protection against a range of COVID-19 outcomes, including against XBB-related sublineages, with the most substantial protection observed against hospital admission and critical illness.
- Liu (2023): The effectiveness of boosters against mortality wanes with time but a booster still provides substantial residual protection six months after receipt. Increasing population hybrid immunity is likely to reduce observed vaccine effectiveness as the pandemic progresses but COVID-19 boosters continue to provide significant benefits in mortality reduction, particularly in high-risk populations such as those aged 65+ years and those resident in aged care facilities.
- Hanberg (2023): A fourth dose of COVID-19 mRNA vaccine reduced the risk of SARS-CoV-2 infection and severe COVID-19 among patients with systemic autoimmune rheumatic diseases using DMARDs during the Omicron era.
- Piekos (2023): COVID-19 vaccination protects against adverse maternal–fetal outcomes, with booster doses conferring additional protection.
- Amir (2023): In adolescents aged 12–15 years, the booster dose decreased confirmed infection rates by 3.3 times (2.8–4.0) compared with in the internal control group.
- Chemaitelly (2023): Boosters substantially reduced infection and severe COVID-19, particularly among individuals who were clinically vulnerable, affirming the public health value of booster vaccination.
- Tartof (2023): The BNT162b2 XBB1.5-adapted vaccine provided significant additional protection against a range of COVID-19 outcomes during a period when XBB sub-lineages were predominant but JN.1 was also co-circulating and rapidly increasing in prevalence. Older versions of COVID-19 vaccines offered little, if any, additional protection compared to the unvaccinated, including against COVID-19 hospital admission, regardless of the number or type of prior doses received.
- Jara (2023): The overall adjusted effectiveness of a second mRNA booster shot is 88.2% (95%CI, 86.2–89.9) against ICU admissions and 90.5% (95%CI 89.4–91.4) against death.
- Payne (2024): During September 2022–March 2023, receipt of bivalent mRNA COVID-19 vaccine was 47% effective in preventing thromboembolic events among immunocompetent persons aged ≥65 years and 51% effective among adults aged ≥18 years with end stage renal disease (ESRD) receiving dialysis, compared with receipt of the original monovalent vaccines alone.
- The HDR UK COALESCE Consortium (2024): Undervaccination was associated with an elevated risk of severe COVID-19 outcomes.
- Decuir (2024): Receipt of an updated COVID-19 vaccine dose provided increased protection against COVID-19–associated emergency department and urgent care encounters and hospitalization compared with no receipt of an updated vaccine dose among immunocompetent U.S. adults during a period of multiple cocirculating SARS-CoV-2 Omicron lineages.
- Lam (2024): Completely vaccinated and patients with booster dose of vaccines did not incur significant higher risk of health consequences from 271 and 91 days of infection onwards, respectively, whilst un-vaccinated and incompletely vaccinated patients continued to incur a greater risk of clinical sequelae for up to a year following SARS-CoV-2 infection.
- Link-Gelles (2024): Receipt of updated COVID-19 vaccine provided approximately 54% increased protection against symptomatic SARS-CoV-2 infection compared with no receipt of updated vaccine. Vaccination provides protection against JN.1 and other circulating lineages.
Systematic Reviews & Meta-Analyses
- Zhu (2022):The pooled results demonstrated a 71% (OR = 0.29, 95% CI = 0.17-0.48) reduction in SARS-CoV-2 infection rates among subjects who received a booster shot compared with those who did not receive a booster shot of coronavirus disease (COVID-19) vaccine. In addition, this analysis emphasized that during the period when the Delta variant was predominant, subjects who received the booster shot showed an 82% (OR = 0.18, 95% CI = 0.13-0.25) reduction in infection rates. Moreover, during the period of dominance of the Omicron variant, subjects who received the booster vaccination displayed a 47% (OR = 0.53, 95% CI = 0.35-0.81) reduction in infection rates.
- Au (2022): For people with delta or omicron related infection, a two dose regimen of an adenovirus vector vaccine with one dose of mRNA booster was 77% (42% to 91%) effective against asymptomatic or symptomatic covid-19 infections, and a three dose regimen of a mRNA vaccine was 93% (76% to 98%) effective against covid-19 related hospital admission.
- Menegale (2023): Booster doses restored VE to levels comparable to those acquired soon after the administration of the primary cycle. However, 9 months after booster administration, VE against Omicron was lower than 30% against laboratory-confirmed infection and symptomatic disease.
- Xu (2023): The risk of SARS-CoV-2 infection, the risk of admission to the ICU, and the risk of death were all higher in the non-booster group than those in the booster group.
- Yang (2023): The efficacy of SARS-CoV-2 vaccines is higher for preventing severe infection and death than for preventing milder infection. Vaccine efficacy wanes over time but can be enhanced by a booster.
- Xu (2023): Inactivated vaccine protection against SARS-CoV-2 infection was moderate, decreased significantly after 6 months following primary vaccination, and was restored by booster vaccination. VE against severe COVID-19 was greatest after boosting and did not decrease over time, sustained for over 6 months after the primary series, and more evidence is needed to assess the duration of booster VE. VE varied by variants, most notably against Omicron. It is necessary to ensure booster vaccination of everyone eligible for SARS-CoV-2 vaccines and continue monitoring virus evolution and VE.
- European Centre for Disease Prevention and Control (2023): Under the Omicron variant, effectiveness of EU-licensed COVID-19 vaccines in preventing any SARS-CoV-2 infection or mild disease is low and only short-lasting after primary immunization, but can be improved by booster vaccination. Vaccine effectiveness (VE) against severe COVID-19 remains high and is long-lasting, especially after receiving the booster vaccination.
- Mohammed (2023): VE against severe Omicron infection following the primary course was 63.6% (95%CI: 57.5–69.7%) at three months, decreased to 49% (95%CI: 35.7–63.4%) within six months, and increased to 86% after the first or second booster dose.
- Rahman (2023): The boosters provided substantial protection against severe COVID-19 outcomes for at least 6 months, although the duration of protection remains uncertain, suggesting the need for a booster dose within 6 months of the third-dose or fourth-dose vaccination.

